Jack and Ben's Birth Story
Jack and Ben are mono-di twins. Mono-di is short for monochorionic, (one placenta) diamniotic (two amniotic sacs). There are lots of risks involved with mono-di pregnancies and they’re monitored closely by perinatologists. Pretty early on, we learned Jack’s share of the placenta was smaller than Ben’s, and he also had a marginal cord insertion, meaning his umbilical cord was attached to the side of the placenta, rather than the center of his share. Both of these things were monitored closely, and Jack was diagnosed with Selective Intrauterine Growth Restriction (sIUGR).
Around week 15, the discordance between the boys’ weights was pretty significant and not improving. At 19 weeks, doctors also began monitoring the blood flow through the boys’ umbilical cords to ensure they were getting what they needed. At that point, Jack’s cord was showing absent diastolic blood flow (two steps forward and stopping, two steps forward and stopping) instead of a continuous flow. Over the next couple of weeks, his cord flow remained absent. Absent cord flow sometimes remains absent, sometimes corrects itself (pretty rare) and often reverses. At 19 weeks, the doctor told us we really needed to make it to 24 weeks and 500 grams so that there was a chance for Jack to survive if they needed to be delivered due to reverse flow.
Weeks 19 through 24 were stressful knowing there was a chance of cord flow reversing and knowing that Jack was not yet big enough to survive outside. At my checkup at 24 weeks + 4 days, the doctor noted reverse flow, and Jack was finally measuring 501g. Dr. Kang, who is absolutely the woman you want taking care of you during this type of situation, hopped up on the ultrasound table with me. She laid her hands on my legs to deliver the news that she was going to admit me to the hospital. She said lots of really nice and encouraging things and I knew she was cheering for us. My friend Alli was with me during this appointment because Justin couldn’t be there, and she was incredible.
Someone came to get us a few minutes later and walked us “the back way” to L&D. After I checked in, they put me in a room in antepartum. I answered a THOUSAND questions about my medical history and they started running vitals. Justin was on his way and Alli and I both kept asking the nurse not to poke me with anything until he could be there. She wasn’t amused, but Justin arrived just a few more minutes before they gave me my first steroid shot to help the boys’ lungs. Shortly after that, they gave me and IV and a round of magnesium as a preventative measure against cerebral palsy. FYI, magnesium is NOT fun!
For the rest of the afternoon and into the evening, I had lots of visitors. The head perinatologist, a doctor from the NICU, a lactation consultant… everyone was trying to prepare us mentally for a 24 week delivery. The difference in survival and health in 24 week babies and 25 week babies is dramatically different. We knew we really really needed to get to 25 weeks at the very least, though we were thankful to have made it to viability at all. That day felt heavy.
I was scheduled for an ultrasound to check cord dopplers the next morning. Before my ultrasound, the nurse had me hooked up to heart rate monitors and a contraction monitor. She noticed Jack’s heart rate was dropping a little bit with contractions (I didn’t even realize I was having) and she kicked things into high gear. She plopped me into a wheelchair and started an IV drip as she was rolling me to the ultrasound room. We call this nurse Super Gabby. Ha! She really was amazing, but her urgency terrified me. She was concerned about placental abruption. (You can look that one up yourself. Let’s just say I’m really really grateful that did not happen.) I held back a panic attack (just barely) through the ultrasound and then we waited and waited for results.
After my ultrasound, they decided to move me to labor and delivery ICU. I didn’t even know I was in ICU until I left, and that was probably a good thing! In L&D, they had me on around-the-clock heart rate and contraction monitoring. I had to stay in the bed except to go to the restroom, and even that was an ordeal with three monitors and an IV pole to take with me. The next two days were brutal — little sleep, no shower, crazy back pain, and basically no food. Each morning, I had an ultrasound that determined the fate of our day — deliver, or get one more day. We prayed hard each morning for another day for the boys to grow and develop.
My bed in L&D ICU. I was on continuous monitoring for about 21 hours straight. I could only get up to use the bathroom.
Friday afternoon, the team decided I would get Saturday “off” — no ultrasound until Sunday morning. They moved me back to my more comfortable room in antepartum. They took my IV out. No more constant monitoring. I got to take a shower AND eat real food. We were SO relieved.
This ultrasound made me cry! It was the first time we had really seen them together in the same image and I just wept over the thought that they had each other’s backs but that they would also be separated soon.
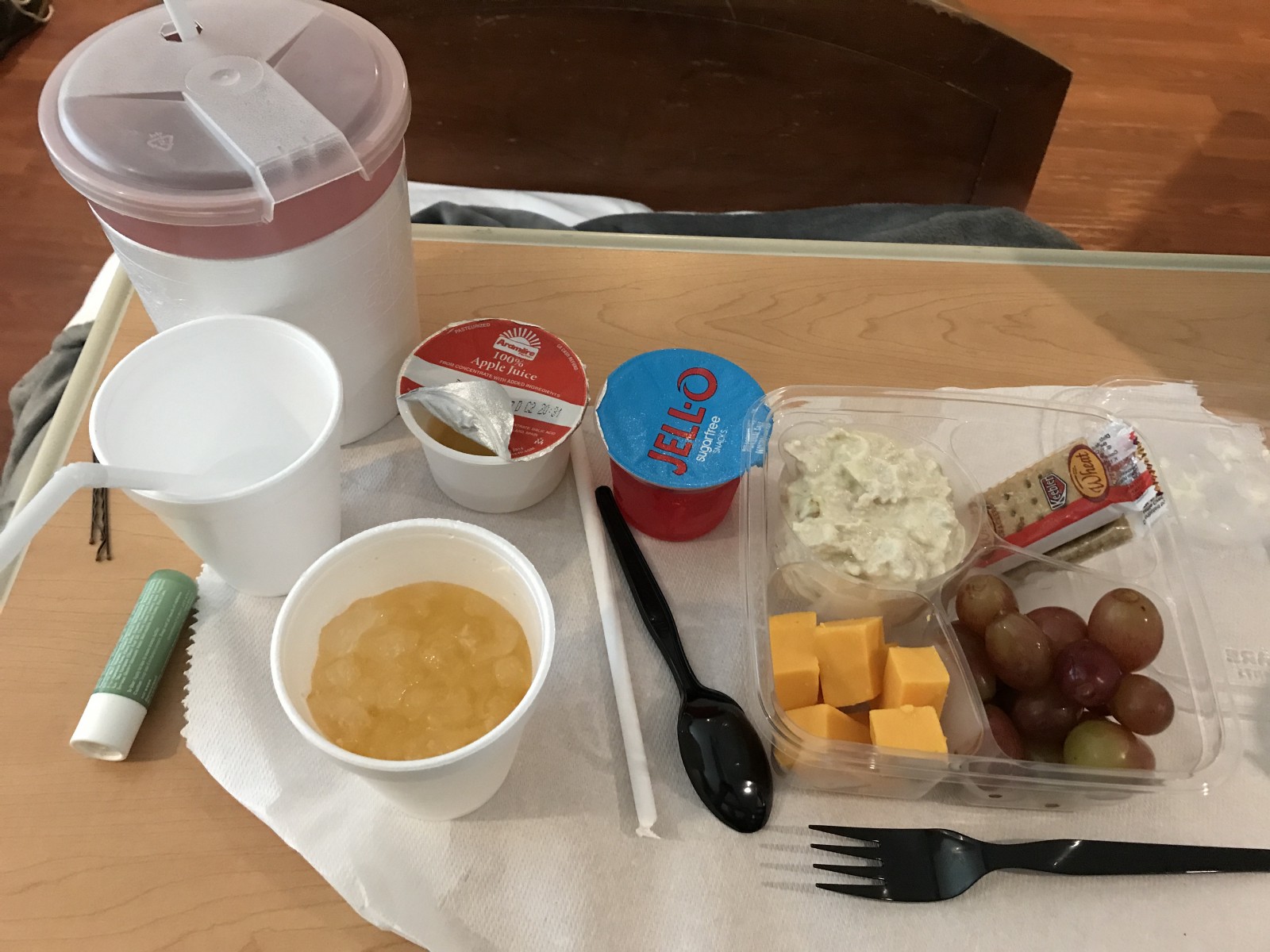
My first “meal” after being NPO for 48 hours.
We woke up Saturday morning decently rested and ordered FIDO for breakfast. I ate, and then they hooked me up to the HR/contraction monitors for 20 minutes. The nurse saw regular contractions and a heart rate dip for my sweet baby Jack, so the doctor ordered an ultrasound. After the ultrasound, Justin and I were sitting and talking about how much the hospital sucked, but that we were so thankful God was giving us more time and that we’d stay there ten more weeks if it meant the boys made it to 35 or even 36 weeks! In the middle of that conversation, the nurse walked back in the room with a gown and a hat and sweetly said, “They’re going to go ahead and section you today.” I remember looking at Justin and not knowing how to feel. Not shocked enough to cry, not at peace enough to say, “Okay, let’s do this.” So instead, I asked if I could take a five minute shower.
So many thoughts ran through my mind as I showered. I could feel every second of my five minutes tick by as I tried to take in the last few moments of being pregnant, remember what it felt like to have my boys inside me. It was so surreal. As soon as I opened the bathroom door, the chaos began. There were three nurses there ready to prep me. As soon as I put on the gown and laid down, one nurse was drawing blood, the other was starting an IV, and the other was shaving my lady bits. I just held Justin’s hand, sort of numb, trying to psych myself up and also keep the anxiety at bay.
The nurse working on my IV set it, flushed it, and tried to push fluid, but it wasn’t working. She flushed it again and it still wasn’t working. I looked at Justin and the nurse and I think the ceiling and finally said, “Um…it’s bubbling in my shoulder….” I could hear it and feel it and knew that was not right. They took it out and sent me down to L&D where another nurse finished prepping me. Thankfully, she was a pro at IVs.
Two female NICU doctors came in and stood at the foot of my bed and explained how they’d care for our babies during delivery. They asked if the boys had names and when we told them we hadn’t finalized yet, they told us we’d better get on it or they’d choose names for us. Their cheerful demeanor eased my nerves just a little bit. After they left, we finalized names. I had wanted to meet the boys before we finalized their names, but I knew there was a chance of something happening to either one of them, and I wanted them to have names when they were born.
Our pastor Gary showed up, and so did my mom. I remember wanting it to be quiet. Silence was they only thing keeping my anxiety at a manageable level. I laid in L&D for what seemed like FOREVER. And I think it was. Eventually, the anesthesiologist came in to talk to me about the spinal. She found out I had eaten breakfast and said “Why are we doing this?! I need to talk to so-and-so. She walked out and came back not even a minute later and said “They ruled it an emergency, let’s go!” Oh okay, way to make a mom feel better. I said goodbye to Justin and tried my hardest to keep it together as the rolled me to the OR.
In pre-op. I was trying everything I could think of to keep my anxiety at bay. Last picture of my bump.
They helped me up on the operating table and put me into position for the spinal. I asked the nurse, Tobie, if I could hold onto her. As they prepped the anesthesia and I held onto Tobie, another nurse named and counted all the tools on the table in front of me. “Spork, seven… 1, 2, 3, 4, 5, 6, 7. Chopsticks, four… 1, 2, 3, 4.” (I have no idea what any of those tools are called) I couldn’t decide if the counting was keeping me sane or making me INsane. The spinal, the thing I was most terrified of, was not as bad as I made it out to be. It was over fast, thankfully.
They laid me down and inserted a catheter. The anesthesiologist started testing to see how the spinal was working. I was terrified of not being completely numb, so I made her double check a few times. She eventually made the doctor show me what tool she was “poking” me with and when I saw it I realized I was NOT feeling pain. As soon as I told her, they started.
Someone said they were going to go get Justin and I said, “Did you already start? He’s going to pass out if you already started.”
Justin came and sat next to me and held my hand. (He did not pass out, for the record.) I felt some pressure and tugging and then heard a tiny, tiny squeak. It sounded like a mouse. My sweet Baby A, Jack, was born at 2:15 PM. They went in for Baby B and he was all the way up in my ribs. The pressure and pulling they did to get him out is truly indescribable. FINALLY, after the longest three minutes ever, sweet and stubborn Baby B, Ben, was born at 2:18 PM.
The incredible NICU team intubated and assessed the boys and Justin was able to take pictures and follow them straight the the NICU as soon as they were stable. I got stitched up and rolled to recovery and Justin re-joined me shortly after.
As I laid in recovery, I remember feeling numb- physically but also emotionally. Eventually, I told Justin I was ready to see pictures of the boys. They were the tiniest babies I had ever seen.
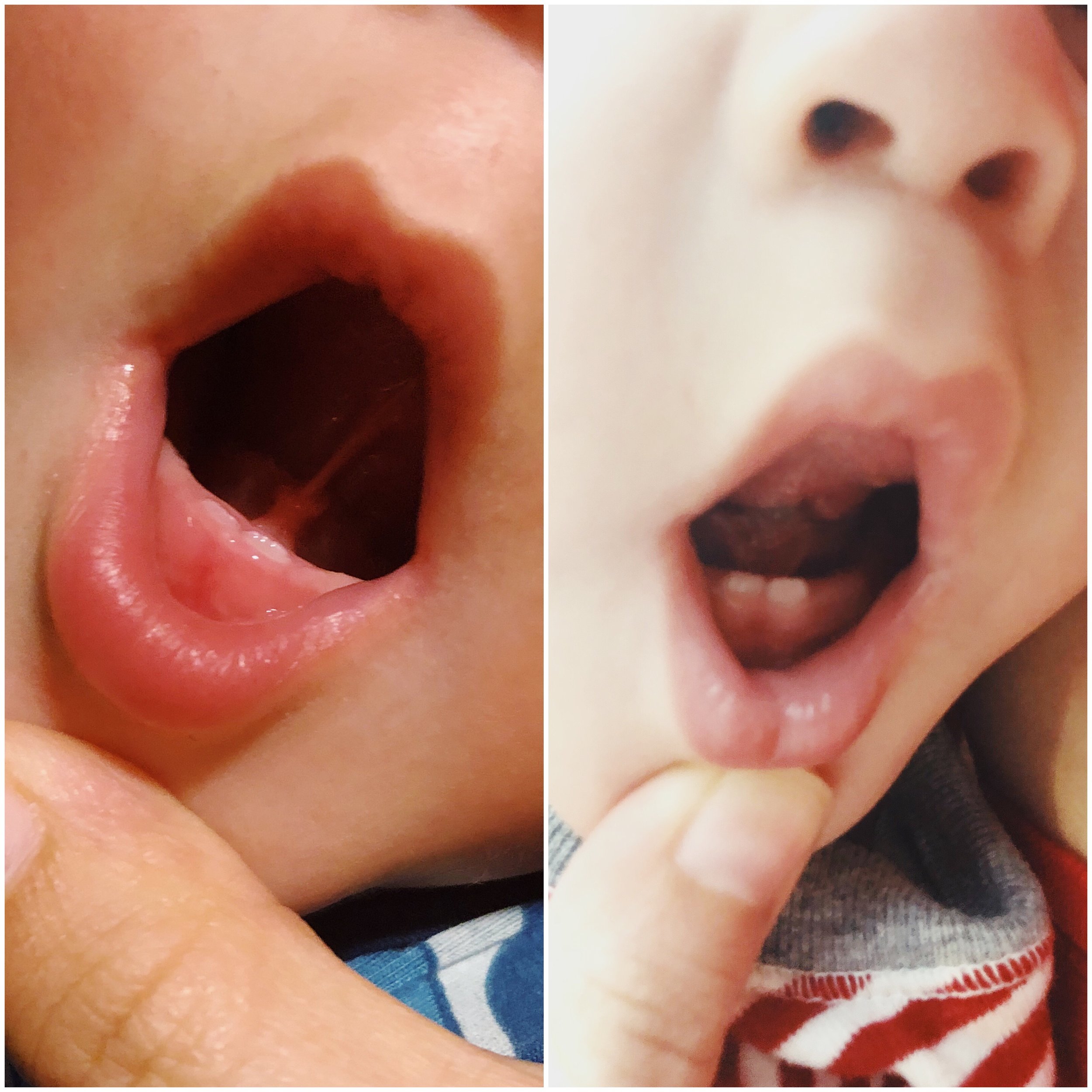
My babies. My fighters. ALIVE. Thank you, Jesus.